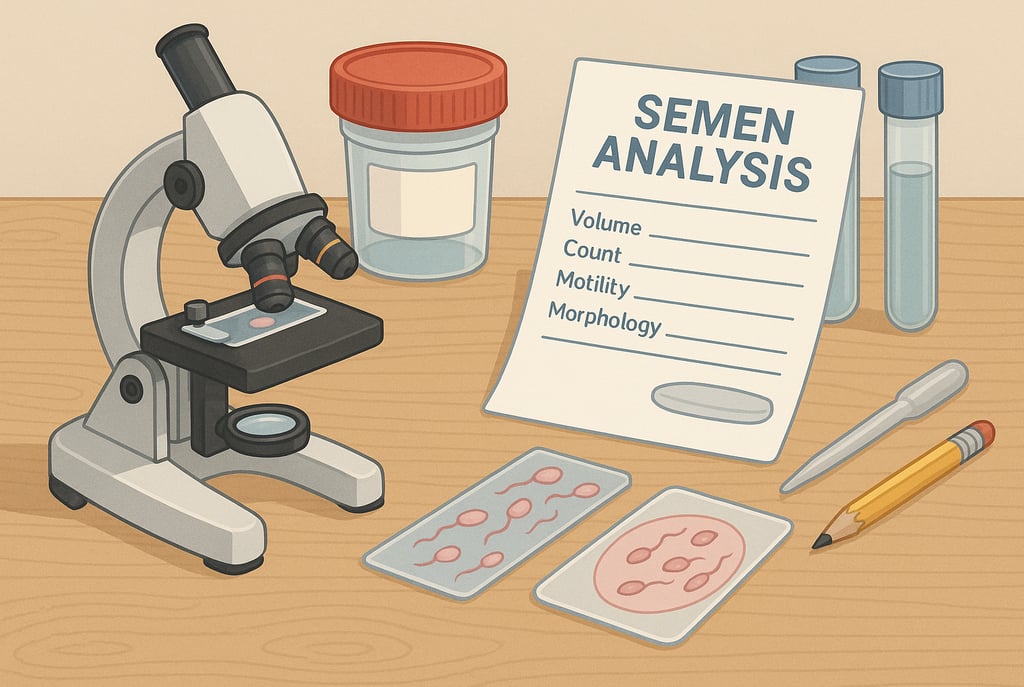
Semen Analysis Explained
Understand your semen analysis: sperm count, motility, and morphology explained — and what the results mean for IVF or ICSI treatment.
DIAGNOSIS & TESTING
When you're starting fertility testing, it’s not just about eggs and ovaries — sperm health matters too. Whether you’re trying to conceive naturally, preparing for IVF, or considering ICSI, a semen analysis is one of the first steps in understanding male fertility.
But what exactly does it test for? And what do those numbers actually mean? Let’s break it down.
What Is a Semen Analysis?
A semen analysis (or sperm test) checks the quantity and quality of sperm in a sample of ejaculate. It’s a simple but important test that can highlight potential barriers to conception or indicate whether assisted reproductive techniques like IVF or ICSI might be needed.
It typically evaluates:
Sperm count (how many)
Motility (how well they move)
Morphology (how they’re shaped)
Volume and pH
Vitality (if enough are alive)
Presence of white blood cells, clumping, or debris
💡 Samples are usually collected after 2–5 days of abstinence and analysed within an hour of ejaculation.
Sperm Count: How Many Are There?
This measures the number of sperm per millilitre of semen and total sperm in the entire sample.
Normal range (WHO guidelines):
Concentration: ≥15 million sperm/mL
Total count: ≥39 million per ejaculate
What low sperm count (oligospermia) might mean:
May reduce chances of natural conception
IVF may be recommended depending on the level
Very low counts might require ICSI, where a single sperm is injected into the egg
Motility: How Well Do They Move?
Sperm need to move forward in a straight line (progressive motility) to reach and fertilise an egg.
Normal range:
Progressive motility: ≥32%
Total motility (progressive + non-progressive): ≥40%
Low motility (asthenozoospermia):
Sperm may struggle to reach the egg
ICSI may be preferred, especially if IVF attempts fail
Morphology: Are They the Right Shape?
Morphology refers to how many sperm have a normal shape, including head, midpiece, and tail.
Normal range (strict Kruger criteria):
≥4% normal forms is considered acceptable
Abnormal morphology (teratozoospermia):
Can reduce chances of natural fertilisation
IVF/ICSI may still work well, as even sperm with unusual shapes can fertilise eggs with assistance
🧠 Only a small percentage of sperm in any man’s sample are perfectly formed — this is normal.
Other Factors in Semen Analysis
Volume: At least 1.5 mL is normal
pH: Typically between 7.2–8.0
Vitality: How many sperm are alive (normal ≥58%)
White blood cells: May suggest infection or inflammation
Clumping: Can indicate anti-sperm antibodies
What If Results Are Abnormal?
It’s important to remember that one test alone doesn’t define fertility. Many clinics recommend repeating the test, since results can vary with illness, stress, or lifestyle.
If results are persistently abnormal, the next steps may include:
Lifestyle changes: Reducing alcohol, quitting smoking, improving diet
Hormone tests or scrotal ultrasound
Referral to a urologist or male fertility specialist
Treatment with IUI, IVF, or ICSI depending on the issue
IVF vs. ICSI: Which One Might You Need?
IVF (In Vitro Fertilisation): Sperm and egg are mixed in a lab dish. Requires reasonably good motility and count.
ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into the egg. Ideal for low count, poor motility, or severe morphology issues.
Your clinic will help you choose based on your full fertility picture.
Related Blog Posts
© 2025. All rights reserved.
