Endometriosis and IVF: What You Should Know
How endometriosis affects fertility and IVF outcomes—plus expert strategies used to improve success rates for each stage of the journey.
DIAGNOSIS & TESTING
Endometriosis can be a confusing and often invisible condition—especially when it comes to fertility. If you’re navigating IVF with a diagnosis of endometriosis, you may be wondering how it will affect your chances of success, what special considerations apply to your treatment, and what you can do to prepare. The good news is that while endometriosis can make conception more challenging, IVF is often a highly effective option.
In this post, we’ll unpack how endometriosis impacts fertility, what IVF protocols can be tailored to this condition, and the latest approaches used to increase your chances of a successful pregnancy.
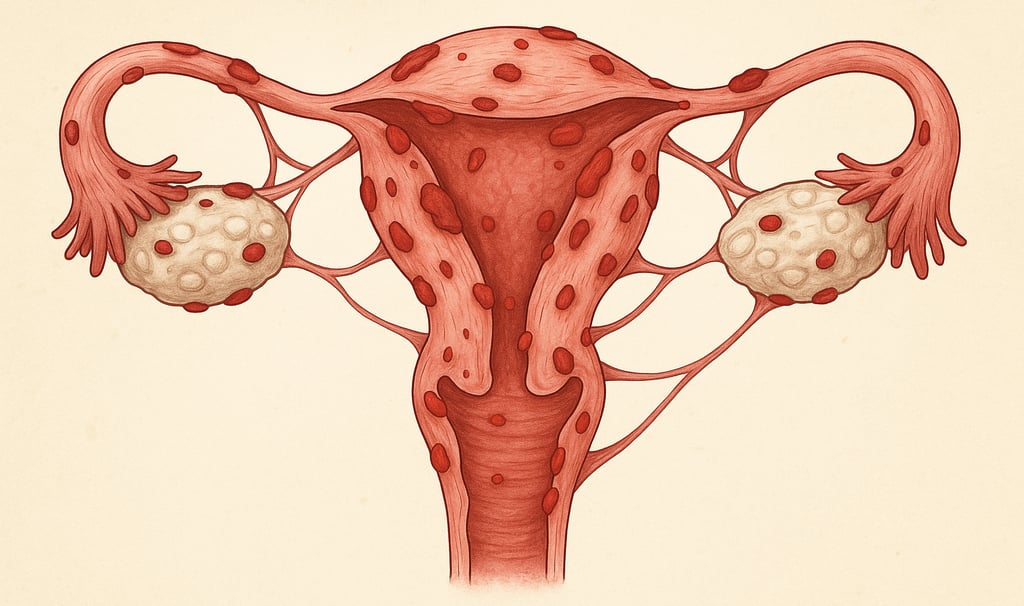
What Is Endometriosis?
Endometriosis is a chronic inflammatory condition where tissue similar to the lining of the uterus (endometrium) grows outside the womb—on the ovaries, fallopian tubes, bladder, bowel, or elsewhere. This tissue behaves like the uterine lining, thickening and bleeding each month, but with no way to exit the body, it causes inflammation, scar tissue, adhesions, and pain.
Common symptoms include:
Painful periods (dysmenorrhea)
Pelvic pain during or after sex
Chronic fatigue
Digestive issues
Infertility
Some people with endometriosis have no symptoms at all—meaning it can go undiagnosed until fertility treatment begins.
How Endometriosis Affects Fertility
Endometriosis can impact fertility in several ways, depending on its severity and location:
Distorted pelvic anatomy: Scar tissue can block or distort the fallopian tubes and ovaries.
Inflamed environment: The inflammatory response can affect egg quality and embryo implantation.
Hormonal disruption: Endometriosis may interfere with ovulation and endometrial receptivity.
Ovarian cysts (endometriomas): These can reduce ovarian reserve or make egg retrieval more difficult.
Even in milder forms, endometriosis can impair fertility without obvious signs on a scan.
IVF and Endometriosis: A Targeted Approach
While endometriosis can reduce natural conception chances, IVF bypasses many of the barriers—particularly if the fallopian tubes are affected. However, your clinic may adjust your IVF plan to improve outcomes.
Here are the most common modifications:
1. Suppression Protocols
For moderate to severe endometriosis, doctors may recommend suppressing the disease before IVF using:
GnRH agonists (such as Zoladex or Synarel) for 1–3 months to lower inflammation
Extended downregulation before starting stimulation
This can help improve implantation rates and reduce pelvic pain during treatment.
2. Mild vs. Aggressive Stimulation
Your ovarian reserve may be lower if endometriosis has damaged the ovaries. Your clinic might:
Opt for a more gentle stimulation if inflammation is a concern
Focus on quality over quantity if the ovarian response is limited
3. Endometrioma Considerations
If you have ovarian cysts, your team may:
Monitor carefully during stimulation
Avoid surgery unless cysts are large or affecting access
Plan aspiration of endometriomas during egg collection in some cases
4. Frozen Embryo Transfer (FET)
Some clinics recommend freezing all embryos and doing a delayed transfer in a calm, inflammation-free cycle—especially if estrogen levels are high or the uterine environment needs more time to recover.
Does IVF Work for Endometriosis?
Yes—many people with endometriosis conceive successfully with IVF, especially when protocols are tailored to their condition. Research suggests:
Success rates for mild to moderate endometriosis are comparable to other IVF patients
Severe endometriosis may slightly reduce success rates, but IVF remains one of the most effective options
Surgery before IVF is not always necessary and should be weighed carefully
Managing Endometriosis Symptoms During IVF
IVF can stir up endometriosis symptoms due to hormonal changes. To ease discomfort and support your body:
Anti-inflammatory diet: Some find relief by avoiding dairy, gluten, or processed foods
Gentle movement: Yoga, stretching, and low-impact activity can reduce pelvic pain
Pain management plan: Speak to your doctor about safe options during treatment
Acupuncture and complementary therapies: These can help reduce pain, improve blood flow, and lower stress
Living with endometriosis adds complexity to your fertility journey—but it doesn’t mean IVF won’t work for you. With careful planning, tailored treatment, and a supportive care team, many people with endometriosis achieve healthy pregnancies through IVF.
If you’re considering or starting IVF, don’t be afraid to ask your clinic how they’ll adapt your treatment for endometriosis—and advocate for the care you need.
© 2025. All rights reserved.
